Wuchereria bancrofti is a filarial nematode worm. Adult Wuchereria bancrofti lives in lymphatic vessels and lymph nodes of human and cause lymphatic filariasis. It causes diseases together with Brugia malayi and B. timori. Various mosquitoes are responsible to spread the filarial worms. It affects over 120 million people throughout the world. If infected people do not take treatment, it can develop into a chronic disease, known as lymphatic filariasis.
Systematic Position
- Phylum: Nematoda
- Class: Secernentea
- Order: Spirurida
- Suborder: Spirurina
- Family: Onchocercidae
- Genus:Wuchereria
- Species:Wuchereria bancrofti
Morphology
It has long, hair-like filiform in shape. Both ends are tapered. The body is white and almost transparent in color. The head end terminates in a small round swelling. The head is surrounded by two rows of 10 sessile papillae. The worm shows sexual dimorphism. The male worm grows up to 4 cm in length with 0.1 mm in thickness with a ventrally curved tail. The tail tip contains 15 pairs of minute caudal papillae with sensory organs while the anal region contains 12 pairs of papillae.

The female worm is longer than the male which can grow up to 10 cm in length with 0.3 mm in thickness. It has narrow and pointed tail end. The most times the adult males and females are often coiled together. The females are ovoviviparous and they can give birth about thousands of offspring, known as microfilariae.
Microfilariae
The lifespan in human body may be up to 70 days. They are colorless and transparent with blunt head and pointed tails. Size is 290 µm × 7µm. The microfilaria has a sheath within which it moves to and fro. In Romanowsky`s stain the embryos shows: (1) Hyaline Sheath. It is an investing membrane round the larva. It is longer than the larval body and projects beyond the extremities. The larva can move forwards and backwards within it. (2) Cuticula and (3) Nuclei. The nuclei extend from the head to the tail end but do not extend up to the tip of the tail. Three clear areas are seen representing the nerve ring, excretory pore (anterior v-spot) and cloaca (posterior v-spot).
Periodicity of Microfilaria: They show nocturnal periodicity, i.e. appear in the peripheral blood at night, mostly between 10 pm and 4pm. At day time they disappear from the peripheral blood and live chiefly in the lung capillaries. It is suggested that the nocturnal periodicity is related with the night-feeding habit of Culex pipiens fatigans.
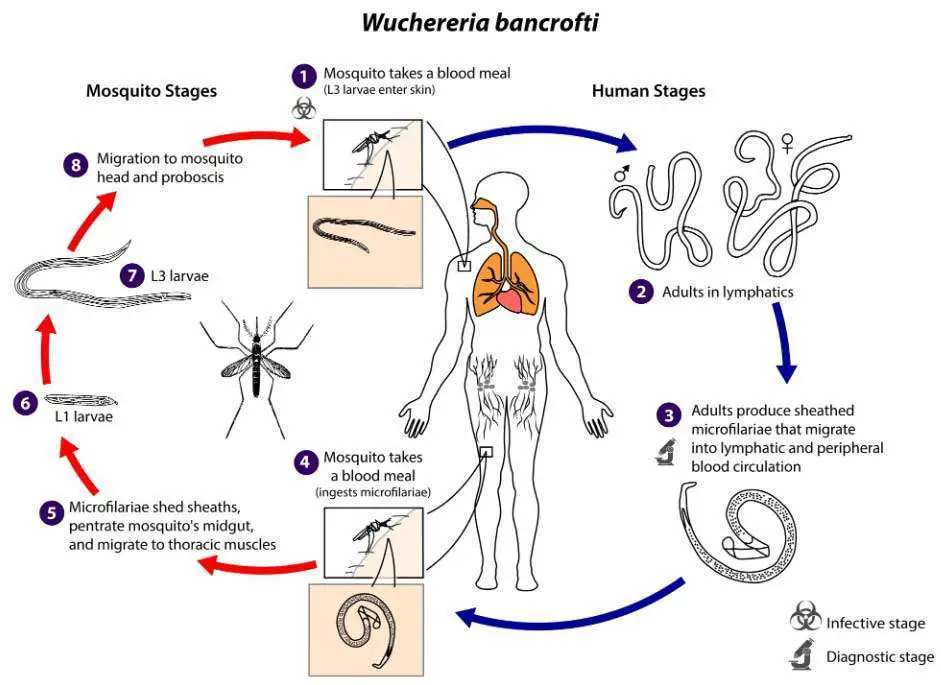
Life Cycle
Wuchereria bancrofti passes its life cycle in two hosts: Human and mosquito.
In Human
Human is the definitive host. The infective larvae are deposited from the proboscis of an infected mosquito on the skin near the site of the bite. Culex fatigans is the most common mosquito. The larvae enter the bite wound or penetrate the skin being attracted by the warmth of the skin. They enter the lymphatic channels, eg. Inguinal or scrotal lymphatics and begin to grow into adults. They become sexually mature in about 18 months. The male fertilizes the female and gravid females give birth to many sheathed larvae. The larvae are known as microfilariae which enter the peripheral blood. The microfilariae are sucked by the female cuticine mosquitoes during their blood meal.
In Female Mosquito
It is intermediate host. A number of species of the genus Culex, Aedes and Anopheles act as intermediate host in which the microfilariae undergo further development and become infective from the man.
Stage of Development
Sheathed microfilariae collect at the anterior end of the stomach of the mosquito after the blood meal. They cast off sheaths, penetrate the gut within 2 hours and migrate to the thoracic muscles. Here they start growing. It becomes sausage-shaped first stage larva with a short spiky tail in about 2 days. In 3 to 7 days, it becomes second stage larvae by one or two moults (sheds cuticle). Metamorphosis is completed by 11th day and third stage larva or infective form is formed. The digestive system, body cavity and genital organs are now fully developed. The infective form enters the proboscis of the mosquito about 14th day. One microfilaria develops into one infective form. During blood-meal the infective larvae are deposited on the skin near the bite.
Infection
Infective larva: Third stage larva formed in the female mosquito.
Transmitting Mosquito: In Bangladesh, Culex pipiens fatigans.
Portal of entry: Skin.
Location site: Lymphatic system of extremities particularly inguino-scrotal region.
Prepatent period: The biological incubation period is about 12 to 18 months. During this period the infective larvae become sexually mature adults. Patent period is the appearance of microfilariae in the peripheral blood.
Pathogenesis and Pathology
Types of Bancroftian or Lymphatic Filariasis
- Classical filariasis is due to adult worm.
- Occult filariasis is due to microfilariae. Tropical pulmonary eosinophilia is a type of occult filariasis.
Classical filariasis
The basic changes in classical filariasis is inflammation leading to periodic attacks of fever.
Lesions
Lymphanitis and lymphadenitis: Lymphatics of epididymis(most common), testes, spermatic cord and lower extremities are commonly involved. Upper extremities may be involved.
Lymphadenitis is most common in the groin. There is intense eosinophilic infiltration. Granulomatous inflammation may occur. The dead worm becomes fragmented or even calcified.
Lymphangitis and lymphadentis are probably due to allaergy, mechanical irritation, metabolites of the worm, toxic products formed from dead worms and secondary bacterial infection, particularly by Streptococcus pyogenes.
Lymphatic obstruction: This is due to mechanical blocking, and inflammatory changes and fibrosis. Ostructed lymphatics become dilated and tortuous and may rupture.
Effects
(a) Hydrocele, lymphoedema of scrotum, penis or vulva, legs.
(b) Varicosity of lymphatic vessels. Rupture of lymphatic varices produces chyluria , chylocele, chylous ascites, chylothorax.
(c) Elephantiasis: It is brought about by recurrent attacks of lymphangitis not less than 10 years. There are hypertrophy and hyperplasia of skin and connective tissue due to fibrotic constriction of lynphatics of the part. Rupture of obstructed lymphatics due to increased lymphatic pressure leads to cellulitis, fibrosis and elephantiasis. Progressive enlargement, coarsening, fissuring of the skin and subcutaneous tissue with warty superficial excrescences develop gradually, causing irreversible elephantiasis. Excessive protein of lymph exudates stimulates connective tissue to excessive growth. Non-pitting solid oedema develops. Elephantiasis of legs and scrotum is common, It also occurs in penis, labia, vulva, breast, forearm.

Clinical Features
1. Symptomatic Filariasis
(a) Due to inflammation. Fever, lymphangitis and lymphadentis. It lasts for a few days, then subsides spontaneously and reoccurs after weeks to months.
(b) Due to obstruction. It takes years(may be even 20 years). Hydrocele, chyluria, elephantiasis and others.
2. Asymptomatic Filarisis in light infection
Occult Filariasis
It is due to microfilariae. Lesions are found in lymph nodes, lungs, liver and spleen. It occurs when microfilariae are destroyed in the tissue and do not reach the peripheral blood. The reaction occurs due to filarial antigen(human or animal). There is massive eosinophilia-30 to 80% and absolute eosinophil count above 3000/cmm. Generalized lymph node enlargement, hepatosplenomegaly and lung symptoms may develop.
Tropical Pulmonary Eosinophilia: This is an occult filariasis. It occurs in patients who are immunologically hyper reactive to filarial antigen, especially those from microfilariae. Pulmonary involvement is marked. Asthma-like respiratory complaints are present. Generalized lymphadenopathy may occur.
Laboratory Diagnosis
1.Demonstration of Microfilariae in (a) peripheral blood particularly at night, (b) Chylous urine, (c) Hydocele fluid.
Methods
- Wet coverslip preparation: Microfilariae are motile.
- Blood film stained with Romanowsky stain (eg. Leishman stain).
- Concentration Technique: Water is added to a sample of blood to lyse red cells. Centrifuged. Films are made with the deposit and stained with Leishman stain.
2. Demonstration of Adult worm in biopsy of lymph node.
- Routine Blood Examination: Eosinophilia (5-15%) in classical filariasis.
- Serology(Immunodiagnosis)
- Immunochromatographic Test: Detects filarial antigen. This rapid test is sensitive and specific.
- ELISA W. bancrofti antigen test.
- Complement fixation test is done with filarial antigen. Dirofilaria immitis is used for preparation of antigen. It may be positive in about 60% cases.
- Indirect immuno-florescence. Positive in 70-90% of cases.
- Skin Test: Intradermal allergic test. It may be positive.
Treatment
Anti-filarial drug treatment is required to get rid of microfilariae. But the drugs have limited effect on adult worms. The following drugs should be used to treat the infected people:
- A combination of albendazole (400 mg) with ivermectin (150–200 μg/kg) with single dose is required where onchocerciasis is co-endemic;
- A combination albendazole (400 mg) plus diethylcarbamazine (6 mg/kg) with single dose in areas where onchocerciasis is non co-endemic; or
- Diethylcarbamazine citrate (DEC) 6 mg/kg alone for 12 days.
Prevention
- Avoidance of mosquito bites;
- Through personal protection measures or community-level vector control and;
- Participation in mass drug administration (MDA) is the best option to prevent lymphatic filariasis.
You may also read: Leishmania donovani: Morphology, Life Cycle, Leishmaniasis and Its Prevention
