Leishmania donovani is a protozoan parasite which belongs to the family Trypanosomatidae under the phylum Euglenozoa. It is an obligate parasite which requires a host for completing their life cycle. It is responsible for the disease, known as leishmaniasis. Over 50 species belong to genus Leishmania were described worldwide; among them about 20 species are responsible to produce human infections, known as leismaniasis. There are many species and subspecies in the genus Leishmania. Some species can produce more than one clinical condition and the same clinical condition can be caused by different species.
The most commons species of Leishmania includes:
- Leishmania donovani
- Leishmania tropica
- Leishmania arabica
- Leishmania aethiopica
- Leishmania orientalis
- Leishmania senegalensis
- Leishmania major
- Leishmania amazonensis
- Leishmania barziliensis
You might also read: Giardia duodenalis: Morphology, Life Cycle, Pathogenesis
Systematic Position of Leishmania donovani
- Phylum: Euglenozoa
- Class: Trypanosomatida
- Order: Kinetoplastida
- Family: Trypanosomatidae
- Genus:Leishmania
- Species:Leishmaniadonovani
Morphology of Leishmania donovani
Leishmania donovani causes kala-azar or visceral leismaniasis. They exists in two stages or forms: (1) Amastigote (Leishmanian-Donovan bdy=LD body) occurs in humans and other mammals and (2) Promastigote occurs in sandfly of the genus Phelotomus. This stage grows in culture media.
Amastigote (LD body): It is non-flagellated, intracellular which lives and multiplies within macrophases and other cells of the mononuclear phagocyte system (Reticuloendothelium system) of mammals. Amastigotes are oval, 2-6×1-3µm with an oval vesicular nucleus and a dark-staining rod-like kinetoplast. There is a rod-shaped parabasal body and a dot-like blepharoplast.
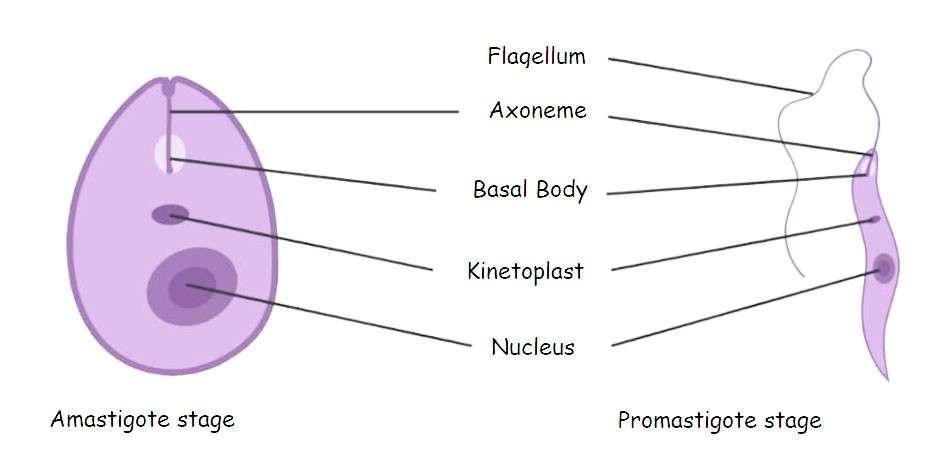
Amastigote and Promastigote stage of Leishmania donovani
Promastigote: It is the flagellated form and occurs only in the gut of the sandflies (inset vector) in nature and also in culture. It is oval or spindle shaped, 10-25 µm in length, nucleus is near the center, kinetoplast is near the anterior end and transversely situated, a single flagellum arises at the anterior end. There is no undulating membrane.
Life Cycle of Leishmania donovani
The life cycle completes in two hosts:
1. Amastigote Form in Human and Other Reservoirs: The infective flagellated promastigotes are introduced with the bite of the infected female sandfly. Then they invade cells of mononuclear phagocyte system and rapidly change to non-flagellated amastigotes. They multiply by binary fission and the cells are packed with the parasites. These infected cells then rupture with the release of amastigotes. The liberated amastigotes then invade fresh cells of mononuclear phagocyte system (reticulo-endothelial system) and the process is repeated. In the peripheral blood, amastigotes may be present inside monocytes.
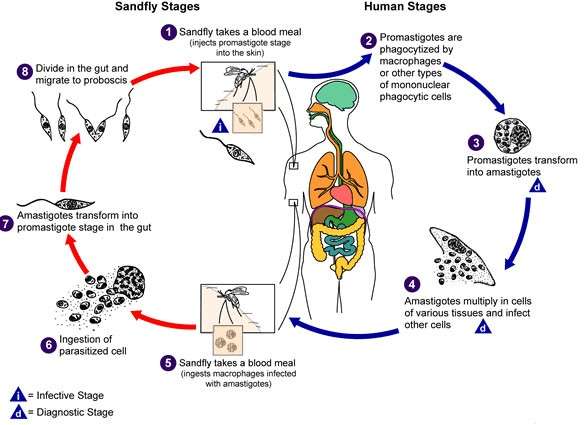
2. Promastogote in Sandfly: The sandfly vector of Bangladesh and India is Phlebotomus argentipes. When the female sandfly feeds blood of an infected person it draws the free amastigote if any and those within monocytes. The amastigotes develop into promastigotes in the midgut of the sandfly. They multiply there by binary fission. Then these motile promastigotes migrate forwards towards anterior part of alimentary canal. Large number of promastigotes form a mass which may block the pharynx of the sandfly in 6 to 9 days. This is known as anterior station development. When the sandfly feeds, the promastigotes are injected into the new host through the bite. In the new host they rapidly change to amastigotes.
Reservoir (Source) of Infection
In Bangladesh and part of the India human is taken as the only source of infection. In Africa rodents are reservoir. In Mediterranean area, Rissia, China and South America canines are reservoir.
Mode of Transmission
(a) Transmission to human occurs during the bite of female sandflies. For Bangladesh and India the vector is Plebotomus argentipes.
(b) During blood transmission.
(c) Congenital infection in uterus.
Virulence Factor
The ability of amastigote to multiply within macrophages is the most important virulence factor. The following factors play important role in its intracellular multiplication.
Glycoprotein 63(gp-63) is a surface component of Leishmania with a molecular weight of 63 KDa. Gp-63 blocks the complement component activities on the surface of promastigote. It also interacts with the monocyte surface receptor. This in turn facilitates the entry of promastigotes within the cytoplasm of monocytes /macrophages. Superoxide dismutase, catalase and glutathione peroxide may have some role. In addition glycoconjugates contribute to the parasite`s resistance to serum complement activity.
Pathogenesis
The infective promastigotes are introduced by the bite of infected female sand-fly. Promastigotes spread from site of inoculation and rapidly change to amastigotes after phagocytosis by macrophages and other cells of reticuloendothelial (mononuclear phagocyte) system especially in spleen, liver, lymp nodes, and bone marrow. The amastigotes multiply within macrophages filling the cytoplasm of the macrophages. The infected cells burst, the released LD bodies are again phagocytosed and the process is repeated producing kala-azar. In some caes, post-kala-azar dermal leishmaniasis occurs 1-2 years after cure of kala-azar.
Type of Leishmaniasis
Kala-azar or visceral leismaniasis:Leishmania donovani causes kala-azar and may develop post-kala-azar dermal leishmaniasis(PKDL).
Cutaneous leishmaniasis of old world like oriental sore, Delhi boil. Causative organisms are Leishmania tropica, L. major and L. aethiopica.
Cutaneous and mucocutaneous leishmaniasis of New World: (a) Cutaneous by L. maxicana (b) mucocutaneous or Espundia by L. braziliensis.
Other Leishmaniasis
A. Cutaneous Leishmaniasis of Old World
1. Leishmania tropica causes oriental sores, or Delhi boil. It occurs in Central and western India and Pakistan but not in Bangladesh. Also occurs in Middle East, Central Asia, West Africa, Sudan and Mediterranean area. The reservoirs of this parasites are doga and gerbils. The morphology is same as that of L. donovani. This is a pure cutaneous infection. The tissues reaction is granulomatous characterized by accumulation of lymphocytes and plasma cells. Then the picture appears tuberculoid. It is followed by ulcer formation. Healing occurs by fibrosis. Amastigote form lives and multiplies within macrophages(histiocytes) in the skin dermis. The rest of the life cycle is same as that of Leismaniasis donovani. The intermediate host is sandfly. The amastigote form may be demonstrated from margin of the ulcer. The material may be cultured in NNN medium. Skin test with antigen prepared from propastigote forms may be positive. Leishmanian or Montenegro reaction is a delayed hypersensitivity skin reaction.
2.Leishmaninia major causes wet oriental sore. Heals in 3-6 months time.
3. Leishmania aethiopica causes oriental sore and diffuse cutaneous lesions.
B. Cutaneous and Mucocutaneous leishmaniasis of New World
1. Leishmania braziliensis causes espundia or mucocutaneous leishmaniasis(American cutaneous leishmaniasis). 80% of cases may develop espundia in the mucosa of nose or mouth. The morphological characters and life cycle are same as those of Leishmania donovani. The intermediate host is sandfly. There is specific uncerating granuloma of the skin and mucocutaneous areas. The parasite (amastigote form) may be demonstrated from the margin of the ulcer by staining of smears and culture of the material in NNN medium. Montenegro leishmanian skin test with antigen of cultured Leishmania braziliensis may be positive.
2. Leishmania maxicana causes chiclero`s ulcer.
Common Symptoms of Leishmaniasis
- nosebleeds
- runny or stuffy nose
- weight loss
- difficulty breathing
- weakness
- fever that lasts for
- enlarged liver
- enlarged spleen
- decreased production of blood cells
- swollen lymph nodes
- bleeding
- other infections
Pathology
The amastigotes of Leishmania donovani live and multiply within cells of mononuclear phagocyte system. The bsic lesion consists of proliferation of the mononuclear phagocytic cells of the spleen, liver, bone marrow and lymph nodes.
Spleen is moderately enlarged in acute kala-azar and may be enormously enlarged in chronic kala-azar. Amastigotes are present within cells of mononuclear phagocyte system.
Liver is enlarged to different extent on the duration of the disease. Kupffer cells are packed with amastigotes. Generalized lymph node involvement may occur even with granulomatous change. Parasitized macrophages may be present.
Bone Marrow shows marjed hyperplasia and contains the amastigotes. Haemopoietic activities are disturbed particularly of the leucopoietic causing neutropenia with leucopenia
Changes in Blood
A. Pancytopenia: There is anaemia, leucopenia and thrombocytopenia.
1.Marked leucopenia with granulocytopenia and relative lymphocytosis. There is almost complete absence of eosinophils.
2. Anaemia is due to: (a) haemolysis (b) Hyperplenism. Red cells are sequestered and destroyed. (c) Ineffective erythropoiesis.
3. Thrombocytopenia
B. Serum albumin is low and serum globulin mainly IgG is raised.
Clinical Features
Incubation period is 1-2 months, maximum up to 10 years.
Fever: (i) Insidious with low grade irregular bouts of fever or (ii) High intermittent fever, sometimes with double rise.
Spelnomegaly (often massive), Hepatomegaly is less marked, anaemia, substantial weight loss, lymphadenopathy (Africa), pigmentation( Kala-azar-fever). Infection is common like tuberculosis, pneumococcal pneumonia. Death occurs due to infection.
Laboratory Diagnosis of Kala-azar
Demonstration of LD body: It is the definite diagnosis.
Specimens
1. Spleen puncture: Spleen puncture material is the best to demonstrate the parasite.
2. Sternal or Iliac crest bone marrow puncture-Second preference.
3. Lymph node puncture
4. Buffy coat of haematocrit. Rarely found.
5. Peripheral blood. Thick film. Rarely found.
Investigations
1.Examination of Stained Smears: (a) Smears are prepared from biopsy material obtained by spleen, sternal, or iliac crest puncture (b) Smear from a buffy coat of haematocrit (c) A thick blood film.
Smears ,are stained by Leishman or Giemsa stain. Intracellular LD bodies (amstigotes) are demonstrated. Amastigotes may be extracellular due to rupture of the cell.
2.Culture: The aspirate material from spleen, bone marrow or lymph node or 1 -2 ml blood(preferably buffy coat) is inoculated into NNN media(Novy,MacNeal and Nicolle medium: the nedium is composed of agar, sodium chloride and defibrinated rabbit blood) and incubated at 220 C for 1-4 weeks. Promastigotes form develops in 1 to 4 weeks. At the end of each week a drop of condensation fluid is examined by:
(a) Motility test: The promastigotes are motile.
(b) Smear stained with Leishmanian stain and the morphology of the promastigote is studied.
B. Blood Picture
White blood cell count: There is progressive leucopenia(Progerssive decrease of leucocyte). WBC count is done every week. There is reltive lymphocytosis, monocytosis and neutropenia. Eosinophils are less or absent.
C. Aldehyde Test:
Nonspecific test: The test is positive due to increase of serum gamma globulin. One drop of formalin (40% formaldehyde) is added per ml serum of the patient. Shaken to mix thoroughly. Addition of an excess of formalin nay give a false-positive result. Solidification with opacity like the white of a hard boilde egg indicates positive result. If these changes occur in 2 to 20 minutes the test is strongly positive. If within 2 hours then it is positive and if in 24 hours it is weakly positive. The test is positive in cases of 3 months duration. The hypergammaglobulinaemia such as cirrhosis of liver, multiple myeloma, schistosomiasis and trypanosomiasis.
D. Serological Tests
Tests detect specific anti-leishmanial antibodies in patient`s serum.
1. DAT (Direct Agglutination Test): DAT is a rapid and reliable test for visceral leishmaniasis and gives positive results in the highest proportion of clinically proven cases. The leishmanial antigen used in the test is a suspension of amastigotes. Detects IgG antibody.
2. K39 antigen strip test: It is a rapid immunochromatographic strip test. Leishmanial antigen is used. Direct IgG antibody to the leishmanial antigen K39.
3. ELISA using a 70 Da antigen.
4. CFT(Complement Fixation Test) with nonspecific antigen of kedrowsky`s acid fast bacillus. Detects IgG antibody.
E. PCR(polymerase chain reaction) is also used for diagnosis.
Immune Responses
1. Antibodies mainly immunoglobulin G is produced against amastigote. This is not protective as most amastigotes are intracellular.
2. Cell-mediated immunity(CMI) is poor in visceral leishmaniasis.
Post-Kala-azar Dermal Leishmaniasis-PKDL
PKDL or dermal leishmanoid is a non-ulcerative cutaneous lesion found in kala-azar patients one to two years after therapeutic or spontaneous cure. It occurs in Bangladesh.
Clinical Lesions: 3 types
1.Depigmented macules particularly on trunks and extremities-earliest lesions.
2. Erythromatous patches. Often butterfly erythema on the nose, cheeks and chin.
3. Nodular lesions. Nodules are soft, painless of varying sizes on skin and rarely on mucous membrane of tongue and eyes.
Laboratory Diagnosis
Biopsy material of nodular lesion and smear stained by Leishman stain, Demonstration of amastigotes of Leishmania donovani confirms the diagnosis. The material may be cultured in NNN media. Prevention of Leishmaniasis
Prevention of Leishmaniasis
There is no vaccine or drugs for treatment of leishmaniasis. It is prevented by avoiding getting bitten by a sand fly. The following step should be followed to prevent being bitten by a sand fly:
- Wearing cloth that covers most of the body. In this case, long pants, high socks and long sleeved shirts are recommended;
- You should use insect repellent to avoid bite from sand fly;
- Spraying with insecticides inside sleeping areas;
- You should sleep on the higher floor of the building;
- You should avoid outdoors between dawn and dusk because sand fly is most active at that time;
- Screen should be used in windows to prevent entrance of sand fly;
You might also read: Wuchereria bancrofti: Morphology, Life Cycle and Pathogenesis
