Hemorrhage is the escape of blood from a blood vessel or the heart. In rupture of the wall of a vessel, hemostatic mechanisms start to control the hemorrhage. A small hemorrhage may have no bad effect but an acute massive hemorrhage threatens the life.
Chronic blood loss produces an iron-deficiency anemia. Hemorrhage may be local or systematic. Systematic hemorrhages occur in hemorhhagic (bleeding) disorders.
You might also read: Sinusitis : Causes, Symptoms and Treatments
Causes of Acute Hemorrhage
- Trauma, eg. Penetrating wounds involving large vessels, bleeding during labour;
- Erosions of blood vessels in chronic peptic ulcer, typhoid ulcer, tuberculosis;
- Varicose veins, eg. oesophageal varices;
- Hypertensions-hemorrhage at sites of arterial weakness;
- Blood vessel diseases, eg. Atheroma, aneurysm;
- Invasion of cancers in blood vessels;
- Hemorrhagic infarction, eg. pulmonary infarction;
Effect of Acute Hemorrhage
The effects depend on the amount and rate of blood loss. A loss of 500 ml (about 10%) of blood has practically has no effect. Sudden acute massive hemorrhage of 1250 ml (about 25%) blood causes shock and a loss of 500 ml may be fetal unless treated. Outcome of a sudden hemorrhage is shown in the following diagram:
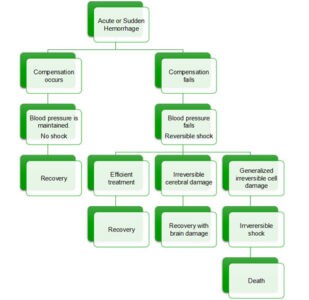
Diagram Showing Outcome of Sudden Hemorrhage
Response after Acute Hemorrhage
Phase-I:
- Immediate syncope may occur;
- Peripheral vasoconstriction with raised blood pressure and rapid pulse;
- Redistribution of blood to vital organs;
- Haematological values: (i) Hb is normal; (ii) PCV-normal, (iii) WBC total count may be raised (iv) platelets may increase;
Phase-II:
- Extravascular fluid passes into capillaries;
- Fluid is retained by kidneys;
- Blood volume may be restored;
- Hematological Values: (i) Hb is decreased; (ii) PCV is decreased ;
Phase-III:
- Lost red blood cells are replaced;
- Reticulocytes increases 5-15%;
You might also read: Economic Importance of Viruses
